Vasectomy side effects: Everything you need to know
- By: Medically reviewed by Kevin Martinez, M.D. — Written by Zawn Villines
- Source: Medical News Today
- Website: https://www.medicalnewstoday.com/articles/327149#long-term-consequences
A vasectomy is a type of permanent sterilization that prevents pregnancy by stopping sperm from entering the semen. The procedure involves cutting or blocking the vas deferens — the two tubes that carry sperm from the testicles to the urethra.
It is a very effective form of male contraception but is not 100% reliable. Approximately 1–2 out of every 1,000 women still get pregnant in the year following their partner’s vasectomy.
Although the procedure is safe, some people may experience pain and other issues afterward.
In this article, we look at a vasectomy in more detail, including common side effects, risks and complications, recovery, and when to see a doctor.
Short-term side effects
It is advisable to abstain from sex for at least a week following a vasectomy.
Below, we list some common side effects of a vasectomy procedure.
1. Pain
Immediately following a vasectomy, a person may feel tenderness, pain, or pressure in the scrotum or pelvic area.
A person should abstain from sex until the pain goes away, which is usually after about a week.
2. Infection
Some people develop an infection at the site of the surgical procedure. The infection can cause intense pain and swelling.
Doctors can prescribe antibiotics to treat the symptoms of a bacterial infection.
3. Bleeding
Excessive bleeding during or after surgery can increase pain and may make additional treatment necessary.
4. Pregnancy
It usually takes about 3 months for the semen to be completely free of sperm.
As a result, it is still possible for a woman to get pregnant immediately after her partner has a vasectomy.
5. Swelling
Swelling and irritation in the scrotum are common. In some cases, the scrotum may look bruised or discolored.
Long-term consequences and risks
Most long-term consequences of a vasectomy are positive. Some people, for example, report improvements in their sex life, which may be due in part to decreased anxiety about unintentionally getting a partner pregnant.
However, there are potential risks following the procedure, including those below.
1. Recanalization
Recanalization happens when the vas deferens grow back to create a new connection, causing the vasectomy to reverse itself.
The sperm are then able to get back into the semen, meaning that the person becomes fertile again.
2. Failed vasectomy
Sometimes, a vasectomy may fail. In this case, a person may need to repeat the surgery or find another birth control option.
3. Regret and uncertainty
Some people may regret having a vasectomy and feel uncertain about whether they might still want children, particularly if they start a new relationship.
Vasectomies are usually reversible, but the likelihood of success depends on the type of vasectomy and the skill of the reversal surgeon, among other factors.
Learn more about vasectomy reversal here.
4. Cancer
The risk of a person getting cancer after a vasectomy is very small.
A 2019 study that followed more than 2.1 million Danish men for 38 years found a small but statistically significant increase in prostate cancer among men who had vasectomies.
Researchers know neither why this risk exists nor whether another independent factor explains the risk.
Penis enlargement surgery: Does it work, and is it worth it?
- By: Medically reviewed by Catherine Hannan, M.D. — Written by Jon Johnson on September 25, 2020
- Source: Medical News Today
- Website: https://www.medicalnewstoday.com/articles/penis-enlargement-surgery
Penis enlargement surgery can involve various procedures, all of which aim to increase the length or girth of the penis. In most cases, people have the surgery for cosmetic reasons.
Although penis enlargement surgery may work in some cases, there is no guarantee that it will be effective, and the procedures carry some risk.
Most people who opt for the surgery have a normal, functioning penis, making the surgery cosmetic. In these cases, the cost can be a barrier for many people.
In this article, we discuss what penis enlargement surgery may involve, its effectiveness and risks, and the costs of the procedure.
What is penis enlargement surgery?
Credit Image: Westend61/Getty Images
Penis enlargement surgery is a procedure that aims to increase the length or girth of the penis.
Surgery may involve the insertion of silicone implants, the transfer of fat cells, or the use of skin grafts to increase the size of the penis. Other approaches may take the form of cosmetic surgery to give the appearance of a longer penis.
The true need for penis enlargement is rare. According to the Urology Care Foundation (UCF), surgery is only necessary if a person has a condition called micropenis. This term describes a penis that is 7.5 centimeters or shorter when stretched.
A penis that functions adequately for both sexual intercourse and urination does not require surgery. The authors of a 2020 review note that the majority of those seeking treatments for penis size have a penis within the normal, functioning range.
How does the procedure work?
There are a few different procedures for penis enlargement surgery, each of which has its own method.
Silicone implants
This type of surgery involves the insertion of a crescent-shaped piece of medical grade silicone under the penile skin to make the penis longer and wider.
Currently, the Penuma procedure is the only penis enlargement surgery that the Food and Drug Administration (FDA) have cleared for commercial use under the 510(k) regulation.
A surgeon first makes an incision above the penis and then inserts a silicone slip through it onto the shaft of the penis. They will shape the silicone implant to ensure that it fits the size and shape of the penis.
Fat transfer
During a fat transfer procedure, the surgeon will remove fat cells from a fatty area of the body and inject them into the shaft of the penis.
They do so by making small incisions into the sides of the penis and injecting purified fat cells into these areas.
Suspensory ligament division
Suspensory ligament division surgery, or ligamentolysis, offers a way to make the flaccid penis appear longer by cutting the suspensory ligament. This ligament attaches the penis to the pubic bone.
During the procedure, the surgeon will sever this ligament and move skin from the abdomen to the shaft of the penis. Although this may make the flaccid penis hang further down, it does not actually increase its size.
The surgeon may also recommend other procedures, such as removing fat from the area surrounding the penis. Doing so may make the penis appear larger, but again, it does not actually change its length.
Other augmentations
Other, less popular augmentations include:
tissue grafts
hyaluronic acid injections
polylactic acid injections
penile disassembly
Does it work?
According to the UCF, almost no method of penis augmentation works.
Currently, the Penuma implant is the only FDA-approved cosmetic surgical pr
What to know about types of penises
- By: Written by Mathieu Rees on November 23, 2020
- Source: Medical News Today
- Website: https://www.medicalnewstoday.com/articles/types-of-penises
The penis is a male organ with functions that include reproduction and urination. As with any body part, no two people have the same penis.
The penis has two main features. The body, or shaft, connects the penis to the abdomen. At the opposite end of the shaft is the glans, or head.
This article lists some common types of penises, categorized primarily by measurement, and provides some related information.
Length
Medical Illustration by Diego Sabogal
Penises come in different lengths when flaccid or erect.
Estimates about average penis length can vary. For example, one 2014 study looked at the penis size of United States males. It found that the average erect length was around 5.6 inches.
However, another article suggests there are issues with many penis length studies, including the fact that participants self-report measurements.
These studies use self-reported data and are therefore subject to bias, which likely fuels the widespread belief that the average penis size is closer to 6 inches. In reality, the average is likely to be lower.
Girth
Penises also have different girths or circumferences.
A 2014 study into the penis size of U.S. males found that the average erect girth was around 4.8 inches.
However, as with penis length, a person should note that many penis girth studies use self-reported measurements, which are known to be fairly unreliable.
Curvature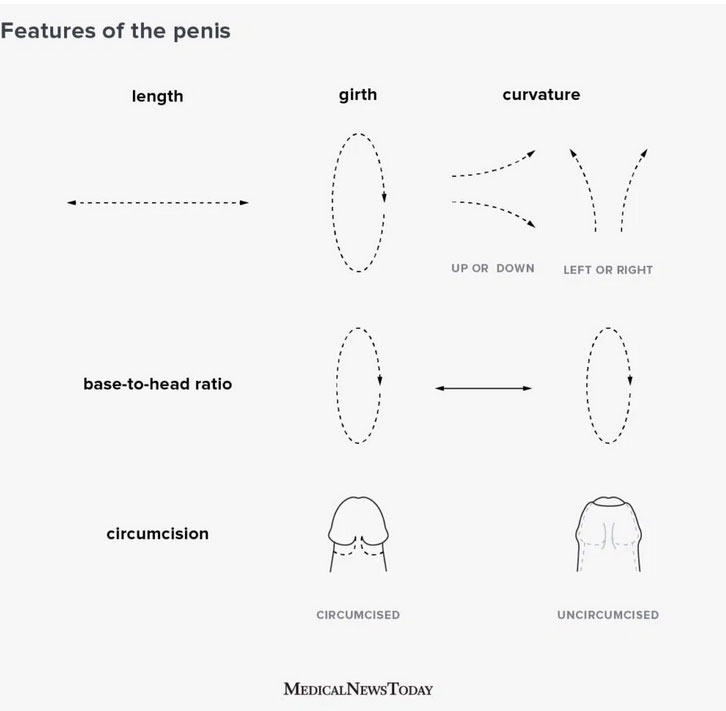
Some penises are completely straight when erect. However, many have a bend or curvature. There are three main types of curved penis. These include penises that:
curve upwards from its base
curve downwards from its base
curve to the left or right
Additionally, some people may have multiple kinds of curvature. For instance, some penises may curve to the left and upwards.
Penile curvatures are common and typically benign. They are rarely painful and do not usually make penetrative sex more difficult.
However, abnormal penile curvature can sometimes be a symptom of Peyronie’s disease. One review lists the following as possible symptoms:
a thickened area, or plaque, in the penile shaft
curvature of the penis during erection
pain in the penis
erectile dysfunction
Scientists are not sure what causes Peyronie’s disease.
One common explanation is that the condition results from mild, recurring trauma to the penis. This can occur during intercourse or masturbation.
Peyronie’s disease can also be due to a rupture in the penis, known as a penile fracture. Genetic factors may also contribute to the development of this condition.
Anybody who suspects they may have Peyronie’s disease should seek medical advice. Sometimes, people with the condition who experience no other issues, such as pain, could still use their penis for sexual activity without needing medical treatment.
In some cases, doctors may recommend surgery to remove the plaque or reduce the curvature in the penis.
Penile melanosis: What to know
- By: Medically reviewed by Cynthia Cobb, DNP, APRN — Written by Jon Johnson
- Source: Medical News Today
- Website: https://www.medicalnewstoday.com/articles/327189
enile melanosis is a rare condition that causes discolored areas of skin on the head and shaft of the penis.
These patches are dark brown and may be slightly or significantly darker than the surrounding skin on the penis.
Penile melanosis does not cause any other symptoms. The condition is not infectious or contagious, and there is no way to pass it on to other people. However, the exact cause is still unknown.
Penile melanosis is generally harmless and does not require treatment. Some people may choose to have cosmetic procedures to remove the spots, though.
In this article, learn more about penile melanosis, including the causes, associated conditions, and treatment options.
What is penile melanosis?
Doctors do not know what causes penile melanosis.
Penile melanosis refers to patches of brown or dark brown skin on the penis. These spots are typically large and flat, with each one appearing alone.
Melanin is one of the main pigments in the skin, and people with more melanin have a darker skin tone. Melanosis refers to a buildup of melanin.
Penile melanosis may also involve other pigment compounds in the skin, such as:
hemosiderin
lipofuscin
ferrous sulfate
As these pigment compounds build up, they can cause a noticeable change in the skin’s color. This hyperpigmentation appears in patches on the penis, rather than affecting the entire penis.
Causes
Doctors are not sure why some people develop penile melanosis. It is simply a buildup of pigment cells within the skin, which can occur in other locations as well.
However, possible risk factors that may increase a person’s chances of developing penile melanosis include:
Age: While penile melanosis can affect people of any age, it mostly appears between the ages of 15 and 72 years.
Genetics: There may be a genetic component to penile melanosis.
Injuries: Previous injury to the penis may play a role, as the formation of scar tissue can lead to hyperpigmentation.
Certain skin treatments: Treatment with certain drugs, such as anthralin or PUVA therapy, may increase the risk of penile melanosis.
Penile melanosis and lichen sclerosus
Penile melanosis may also have a link to another uncommon skin condition called lichen sclerosus.
Lichen sclerosus causes thin, pale patches of skin, usually in the genitals or hands. A 2017 case study of an older man found an association between the penile melanosis and lichen sclerosus on his penis.
However, this does not mean that one of these conditions causes the other. It simply suggests that there may be a link between them.
Penile melanosis and cancer
Some people may worry that discolorations such as these will lead to melanoma, a form of skin cancer. Penile melanoma is very rare.
Penile melanoma may cause darker spots of skin similar to those of penile melanosis, but typically just on the head of the penis. These may grow, change color, and bleed.
WHO And UNAIDS Recommend Male Circumcision
- By: World Health Organization
- Source: World Health Organization
- Website: https://www.sciencedaily.com/releases/2007/03/070328110815.htm
WHO And UNAIDS Recommend Male Circumcision As A Step Towards HIV Prevention
n response to the urgent need to reduce the number of new HIV infections globally, WHO and the UNAIDS Secretariat convened an international expert consultation to determine whether male circumcision should be recommended for the prevention of HIV infection.
Based on the evidence presented, which was considered to be compelling, experts attending the consultation recommended that male circumcision now be recognized as an additional important intervention to reduce the risk of heterosexually acquired HIV infection in men. The international consultation, which was held 6-8 March 2007 in Montreux, Switzerland, was attended by participants representing a wide range of stakeholders, including governments, civil society, researchers, human rights and women's health advocates, young people, funding agencies and implementing partners.
"The recommendations represent a significant step forward in HIV prevention," said Dr Kevin De Cock, Director, HIV/AIDS Department in WHO. "Countries with high rates of heterosexual HIV infection and low rates of male circumcision now have an additional intervention which can reduce the risk of HIV infection in heterosexual men. Scaling up male circumcision in such countries will result in immediate benefit to individuals. However, it will be a number of years before we can expect to see an impact on the epidemic from such investment."
There is now strong evidence from three randomized controlled trials undertaken in Kisumu, Kenya; Rakai District, Uganda (funded by the US National Institutes of Health); and Orange Farm, South Africa (funded by the French National Agency for Research on AIDS) that male circumcision reduces the risk of heterosexually acquired HIV infection in men by approximately 60%. This evidence supports the findings of numerous observational studies that have also suggested that the geographical correlation long described between lower HIV prevalence and high rates of male circumcision in some countries in Africa, and more recently elsewhere, is, at least in part, a causal association. Currently, 665 million men, or 30 % of men worldwide, are estimated to be circumcised.
Male circumcision should be part of a comprehensive HIV prevention package
Male circumcision should always be considered as part of a comprehensive HIV prevention package, which includes
the provision of HIV testing and counselling services;
treatment for sexually transmitted infections;
the promotion of safer sex practices; and
the provision of male and female condoms and promotion of their correct and consistent use.
Counselling of men and their sexual partners is necessary to prevent them from developing a false sense of security and engaging in high-risk behaviours that could undermine the partial protection provided by male circumcision. Furthermore, male circumcision service provision was seen as a major opportunity to address the frequently neglected sexual health needs of men.

